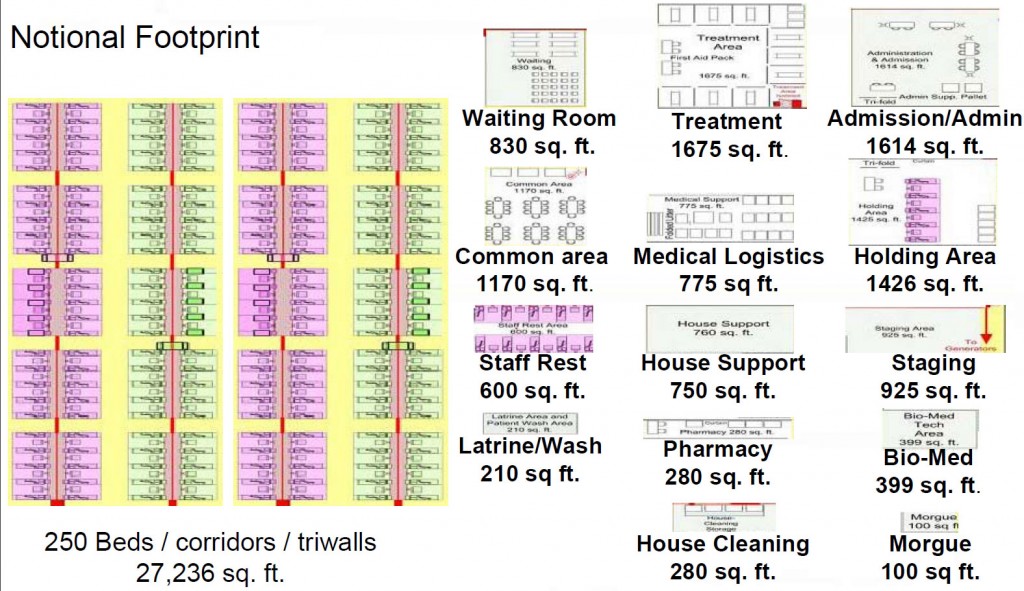
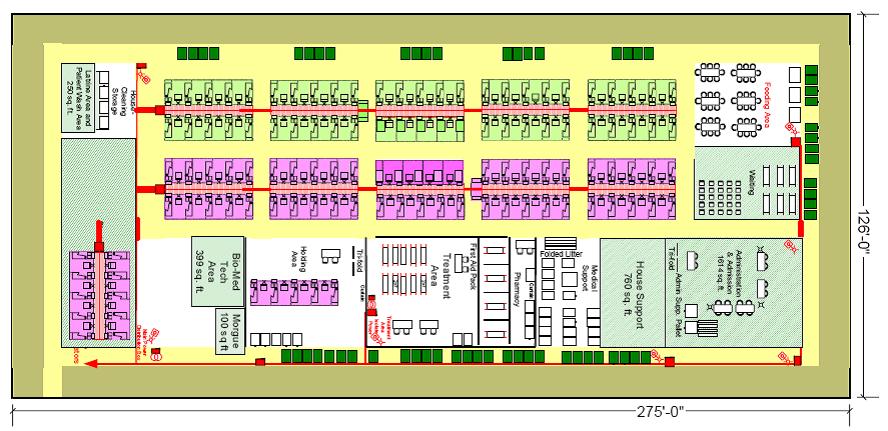
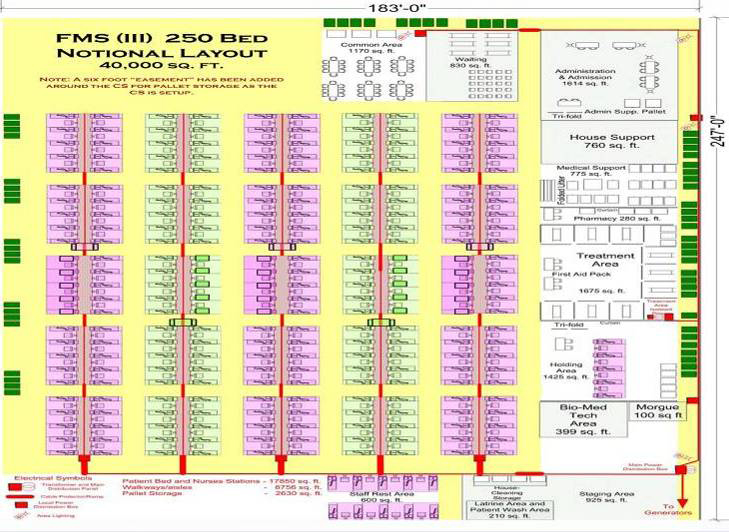
The layout of a facility providing TMTS services will depend on the type of space, the functionality and the type of services that will be provided. These layouts should serve as a guideline, but will need to be tailored to the situation (L-shaped, multiple floors, etc.). Allocation of space will depend on bed capacity needed, patient acuity, and medical logistics support. It is estimated that a 50-bed capacity TMTS will require approximately 9,000 square feet while a 250-bed capacity TMTS will require approximately 40,000 square feet. As a reference, American high school gymnasiums have a minimum space capacity of 7,300 square feet. Additional space needs in TMTS facility layout will depend on the total size and number of beds needed to respond to the emergency. An infectious disease scenario requires specific distance between beds, and ideally barriers between patients. Refer to infectious disease experts for recommendations.
A twin bed is approximately 3.5′ X 6.5′ which requires aisles to be 2.5’ (wide enough to accommodate wheel care or stretcher). A general calculation can be made of the # number of beds x 54 sq ft = amount of space needed for minimal patient care. This does not include the space needed for logistics, supply, intake, discharge, or staff break/rest area. The space needed for the patient bed area is the main driver of the TMTS space requirements as support areas generally remain the same dimensions.
- This spacing may need to be adjusted during an infectious disease scenario to follow health department recommendations.
The main goal of the general layout should be to maximize patient flow and provide efficient patient management services. Keep in mind the following main guidelines:
- Traffic patterns should allows rapid access to every area with minimal cross-traffic
- Patient bed areas should be centrally located to all functional support
- Allow at least two feet of clear floor space between heads of beds
- Side by side cot spacing should be not less than 2 feet with 4 feet being ideal. Consider leaving space between the head of each bed to store disposable/nondisposable medical supplies or patient belongings. Modular plastic bins or similar storage solutions would be ideal.
- Admission and disposition area is focus of initial patient presentation and disposition and should be located at main entrance if possible.
- Support and storage areas are best arranged around periphery or upper floors of the building.
Layout objectives:
- Patient flow should allow rapid access with minimum cross-traffic. One-way traffic and signage should be used. Also consider duct tape/painter’s tape for easy definition of pathways and traffic flow. See example.
- Beds within the nursing subunits should be organized in a grid. This allows clinicians to make rounds and know exactly where to find a patient (e.g. bed B3).
- Visitor/patient public areas should not traverse the clinical areas to assure patient privacy.
- Nursing sub-units should be centrally located and in close proximity to the admissions/registration area to assist in managing high volume intake periods.
- Patient reception entrance should be well lit and clearly identified using signage in multiple languages and near the patient/ambulance drop-off. A good resource for signs translated into multiple languages can be found here: http://www.healthinfotranslations.org/about.php.
- Admissions/Registration should be located near main entrance and on ground floor for ease of patient access.
- Communications and logistics (communication, support, and supply) is a separate area but easily accessible to nursing sub-units, and should be arranged around the periphery.
- Staff support areas will be located separately.
- Multiple restrooms should be easily accessible.
- Doorways and Corridors
- Must be sufficient size to accommodate wheeled stretchers and wheelchairs with attached intravenous poles and other equipment with ease.
- Must be wide enough to allow cross-passage of personnel and equipment (e.g. two wheeled stretchers/ wheelchairs/delivery carts) to enter, exit, and maneuver.
- Other areas (e.g., counseling areas, pharmacy, child care, etc.) may be utilized yet should not impede patient flow
- Admissions/Registration
- Communications
- Hand-washing/sanitizing stations.
- Nursing subunits
- Multipurpose family/visitor area
- Multipurpose staff area
- Pharmacy and medication preparation – this area will need to be secured.
- Supply storage and distribution
- Staff workstations
- Support services (storage, bathrooms, utility)
- Food services
- Maintenance
- Transportation dispatch and equipment
- Secure area (for patient valuables, deceased persons’ belongings)
- Temporary morgue
Vehicle traffic:
- Flow should allow rapid access with minimum vehicle traffic constraints. One-way traffic and signage should be used.
- The main car parking lot should be well lit and situated as close to the main entrance as possible. This lot lot should be used for patients, their relatives. Consider denoting a separate reserved or secured area for staff.
- Should include areas for private vehicles/taxis for pick-up/drop-off of patients including those with limited mobility. This area will need to be well marked with appropriate signage.
- Should provide ambulance/buses/alternate transportation area that is easily accessible for transferring patients.
- Should include an equipment and supply loading and unloading zone that is accessible to the patient care area.
- Other parking should be designated for:
- Law Enforcement
- Transportation vehicles not in use
- Logistical resupply vehicles
- Ambulances that are not in use
- Taxis and private vehicles waiting to pick up patients